 Anti yeast therapy
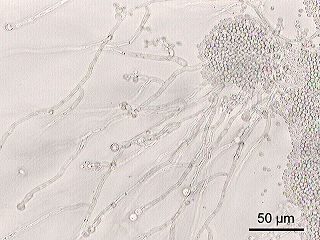
Anti yeast therapy There is some evidence that candida albicans may cause or exacerbate behavior and health problems in autistic individuals. The only physical symptoms are vaginal yeast infections and thrush (white patches in mouth).
An overgrowth of candida albicans causes toxins to be released into the body which are known to impair the central nervous system and the immune system. Some of the behaviors related to this are, confusion, hyperactivity, short attention span, lethargy, irritability, and aggression. Reported health problems can include headaches, intestinal problems,(constipation, diarrhea, flatulence), distended stomach, excessive genital touching in infants and young children, cravings for carbohydrates, fruits and sweets. Unpleasant odor of hair and feet, acetone smell from mouth, and skin rashes.
Candida overgrowth is often attributed to long term antibiotic treatments. It has been reported that some children whose autistic tendencies surfaced at 18- 24 months had been continuously treated with antibiotics to control chronic ear infections. The treatment doesn't cure autism, but is helpful for some autistic children.
Some clinicians believe that autistic symptoms are made worse by the overgrowth of Candida albicans, a yest-like fungus present everywhere. Overgrowth is made possible by a dysfunctional immune system. A healthy immune system would keep the Candida in check.
The "leaky gut" theory of autism implies that withdrawing gut allergens and treating yeast overgrowth, should help the GI tract to return toward normal and autistic symptoms improve.
Many children afflicted with autism have had frequent ear infections as young children and have taken large amounts of antibiotics. These are thought to exagerate the yeast problem. Other possible contributors to Candida overgrowth are hormonal treatments; immunosuppresant drug therapy; exposure to herpes, chicken pox, or other "chronic" viruses; or exposure to chemicals that might upset the immune system. There is an increased probability, that a "general" environmental factor affecting our immune systems (i.e. ozone layer depletion, "toxic" chemicals, etc.) may be operative, affecting many children and adults.
Because it is impractical to expect anyone to stay on a totally yeast-free diet, ongoing medication, anti-fungal supplements, and avoidance of sugars are often used to control Candida. Even with the use of anti-fungal drugs, it is still important to limit sugar, because yeast grows 200 times faster in the presence of sugar.
If a potent anti-fungal such as Diflucan or Nizoral is used, it can be assumed that within 1 - 2 months most all of the yeast will die off. When Nizoral or Diflucan is used, some experts say that within 7- 12 days patients can experience "die off" symptoms. This consists of either a "sensitization" reaction to "products" released when the yeast is killed, or the release of "formaldehyde" like products or other potentially toxic derivatives during yeast death, that can contribute to negative symptoms in a patient, including hyperactivity, gastrointestinal distress, and irritability. Die-off usually lasts about 7-14 days and after that time the change in the child is reported as sometimes dramatic. If the die-off does not end in 14 - 17 days, the anti-fungal medication is usually changed.
If the treatment is successful for autistic children, usually eye-contact improves and the child seems more aware and less"foggy." Anecdotal reports claim that the frequency of inappropriate noises, teeth grinding, biting, hitting, hyperactivity, and aggressive behavior decreases. The child acts less silly and shows less inappropriate laughter.
The antifungals, Nizoral and Diflucan, are usually monitored with liver function tests drawn every 1-3 months, since these drugs can cause liver damage. Some physicians stop pharmacological antifungals at six months because of postulated effects on the adrenocortical axis. Then, some will switch to Amphotericin B, which has recently been licensed as an oral liquid in the United States, and can be legally compounded by pharmacies in the U.S.
If the antifungal therapy is stopped, and the body's immune system is still sub-optimal, the yeast is thought likely to return. Many believe treatment must be continued for 4 - 6 months to maintain gains obtained from yeast elimination. Stopping treatment after only one month is thought to allow yeast to return in perhaps even more resistant forms.
Probiotics for keeping healthy intestinal flora include:
Related:


No comments:
Post a Comment